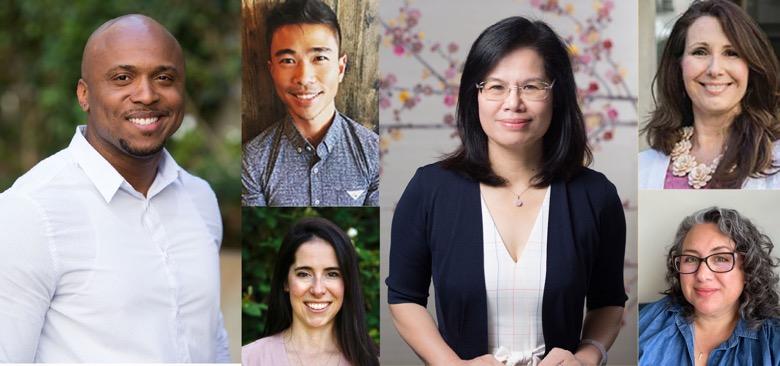
UCSF School of Nursing alumni and faculty have played pivotal roles in responding to the COVID-19 pandemic. Among these impactful changemakers are (from left), Orlando Harris, Glenn-Milo Santos, Sarah Berger, Jian Zhang, Gina Shuler and Desiree Espinoza.
25 COVID Changemakers
Nurses have been leaders in the battle against the coronavirus since the beginning of the pandemic. Working long hours in ICUs and emergency rooms, they delivered quality care to patients. They launched research studies to better understand the pandemic’s impact and helped devise solutions to improve health care, widen health access and shape policy. They transitioned academic programs to remote delivery to ensure the preparation of future nursing leaders continued, without interruption.
Meet 25 UCSF nursing faculty and alumni — the School's #COVIDChangemakers — who have made a remarkable difference during this pandemic through their commitment, innovation and leadership.
 Ifeyinwa Asiodu Ifeyinwa Asiodu, PhD (’14), MS (’12), FAAN, Assistant Professor
Ifeyinwa Asiodu Ifeyinwa Asiodu, PhD (’14), MS (’12), FAAN, Assistant Professor
Since the start of the pandemic, Ifeyinwa Asiodu has explored the impact of COVID-19 on mothers and birth workers of color. Asiodu co-developed and led the COVID-19 Birth Worker Relief Fund. Under her leadership, this effort raised over $350,000 and disseminated 150 one-time grants to birth workers of color providing perinatal services during the pandemic.
She also collaborated with a research team that found that the plasma and milk from COVID-19 vaccinated mothers contained potent antibodies to the virus and the women did not report serious side effects. This work builds on previous research examining more than 250 infants to understand the birth outcomes for women who tested positive for COVID-19. Asiodu continues to lead the COVID-19 and Infant Feeding Study, examining perinatal and infant feeding experiences of California-based women and birthing people during the COVID-19 pandemic.
Sarah Berger, MS ’18, CNS, CCRN  Sarah Berger
Sarah Berger
A year before COVID-19 entered the vernacular, Sarah Berger spearheaded an initiative to train UCSF nurses on a new manual proning method. That training proved invaluable during the pandemic as many COVID patients required proning while in the ICU.
Since spring 2020, Berger has managed multiple efforts: providing patient care, preserving PPE, coordinating testing supplies for inpatients, adapting nurse workflows, and adjusting practices frequently based on supply chain shortages. In January 2021 when UCSF ICUs were at capacity with COVID patients, Berger returned early from maternity leave to help with the surge.
“The most challenging part at the beginning of the pandemic was keeping up with the constant changes: changes in patient care guidelines and recommendations, changes in supply chain shortages and needing to adapt nursing practices. It felt like every week we had to revamp something,” she said. “The most rewarding part has been seeing long-term patients make full recoveries and return home to their families. It has also been very rewarding to see our ICU staff come together to overcome incredible challenges over the last 18 months.”
 Abraham Brody Abraham Brody, PhD ’08, RN, FAAN
Abraham Brody Abraham Brody, PhD ’08, RN, FAAN
A geriatric and palliative care consultant at NYU Langone Health, Ab Brody was redeployed as a nurse practitioner to help treat COVID-19 patients during the spring 2020 surge in New York City. It was a different role for him. Instead of being a consultant offering an external expert opinion, he was now on the front lines, delivering day-to-day patient care and management as part of an inpatient COVID-19 medicine service. For him, the reason he agreed to help at the front lines was straightforward: “There was a need, plain and simple, and we all have to chip in.”
When he is not treating patients, Brody is an associate professor at the NYU Rory Meyers College of Nursing and associate director of the Hartford Institute for Geriatric Nursing where he trains and mentors students. He is also the principal investigator for two NIH-funded clinical trials aimed at improving the quality of care and quality of life for persons living with dementia and their care partners and is the Pilot Core Lead of the NIA IMPACT Collaboratory.
Dena Bushman, MS ’12, RN, MPH  Dena Bushman
Dena Bushman
Dena Bushman was an Epidemic Intelligence Service Officer with the Centers for Disease Control (CDC) at the New York City Department of Health from July 2019 to July 2021. During this period, Bushman and her team conducted sentinel surveillance and genomic sequencing of SARS-CoV-2 to determine geographic origin, assessed risk factors for in-hospital death with COVID-19 among people ages 21 to 64 and investigated post-COVID conditions. Bushman was also deployed to Wisconsin as the medical epidemiologist to evaluate a SARS-CoV-2 antigen test and to an emergency intake site for 1,500 unaccompanied minors at the U.S.-Mexico border where she served as team lead to oversee the implementation of infection prevention and control measures. Her work resulted in critical findings, which were disseminated in nine publications and numerous scientific presentations. She now serves as a medical epidemiologist with the CDC assigned to Maine Center for Disease Control & Prevention.
 Garrett Chan Garrett Chan, PhD ’05, RN, FAAN, Associate Professor
Garrett Chan Garrett Chan, PhD ’05, RN, FAAN, Associate Professor
Garrett Chan’s ingenuity during the pandemic expanded COVID-19 vaccine access to thousands. He created VaxForce, a volunteer registration and matching system that allows health care professionals and students to staff vaccination events throughout California. VaxForce focuses on partnering with community-based organizations and vaccination events in under-resourced communities and communities of color. Volunteers utilizing VaxForce’s platform have administered more than 5,800 doses of the COVID-19 vaccine in 34 vaccination events across California and about four of every five vaccine recipients were people of color. Chan’s efforts were recognized by Johnson & Johnson in its “Meet 15 Nurses Who Disrupted Healthcare Through the COVID-19 Pandemic.” In addition to being an associate professor at the School of Nursing, Chan is president and chief executive officer of HealthImpact, a California nursing workforce and policy center.
Jyu-Lin Chen, PhD (’02), RN, FAAN, Professor  Jyu-Lin Chen
Jyu-Lin Chen
Nurses play a vital role in responding to urgent situations such as the pandemic. Jyu-Lin Chen has been leading multiple studies aimed at advancing nurse leaders’ knowledge and improving patient care. Among these, one study that published earlier this year identified how to increase nurse leaders’ knowledge and confidence in disaster management. In addition, she is currently leading a research team that is examining UCSF’s COVID-19 patient hotline, which is headed by nurses and nurse practitioners and has played a critical role in serving patients’ needs during the pandemic. The study examines how this model has influenced patient compliance and their health, as well as identify risk factors and vulnerable and marginalized populations. Chen’s team includes fellow researchers Rosalind De Lisser, Thomas Hoffmann, Hannah Jang (alumna), Chen-Xi Lin, Jerry John Nutor and Mijung Park.
 Leslie Dubbin Leslie Dubbin, PhD (’14), MS, (’09), RN, Assistant Professor
Leslie Dubbin Leslie Dubbin, PhD (’14), MS, (’09), RN, Assistant Professor
Leslie Dubbin is leading a California-wide study, along with professor Janet Shim, to shed light on the experiences of RNs caring for COVID-19 patients. Their findings, thus far, reveal that many hospitals and health systems have discontinued many of the health and wellness support services offered to nurses when the pandemic began. They also found that nurses’ initial fear of caring for COVID-19 patients has ebbed due to standardized infection prevention standards, adequate quantities of personal protective equipment, and the availability of vaccines. Still, the emotional toll of the initial surge has prompted many nurses, particularly those in critical care, to reevaluate their careers and future trajectories. Findings also reveal many nurses are viewing the future with increasing worry because of the politicization of the pandemic. Nurses report frustration at the number of unvaccinated patients being admitted to hospitals for something that is now viewed largely as preventable.
Jamilah Dula-Crawford, MS, RN, Clinical Instructor  Jamilah Dula-Crawford
Jamilah Dula-Crawford
It was in April 2020 — the start of the pandemic — when UCSF issued an urgent call for health care volunteers to provide medical support to the Navajo Nation, which was experiencing a disproportionate number of COVID-19 cases. Jamilah Dula-Crawford, a UCSF Health nurse and a clinical instructor at the UCSF School of Nursing, did not hesitate. She joined a team of 14 nurses and seven physicians who flew to Arizona and New Mexico, where the group spent six to eight weeks delivering urgent medical treatment in high-volume hospitals that serve Navajo patients. (Dula-Crawford is pictured at right at San Francisco International Airport as the team waited to board a flight to help the Navajo Nation.)
“Throughout this pandemic and in these unprecedented times, it was a truly humbling experience for me to witness how dedicated our health care providers have been to taking care of patients, not to mention how resilient and persevering the Navajo have been in navigating these challenges,” Dula-Crawford said. “Nursing has a profound ability to impact lives around the world, and this experience and this pandemic have certainly reinforced just how vitally important that role is.”
 Desiree Espinoza Desiree Espinoza, MS ’17, RN, CPNP-PC
Desiree Espinoza Desiree Espinoza, MS ’17, RN, CPNP-PC
In January 2021 when La Clinica partnered with Contra Costa County to offer mobile COVID-19 testing to hard-to-reach residents, Desiree Espinoza was tapped to develop a mobile team. With 10 staff and dozens of volunteers, the mobile unit provided free testing at La Clinica sites across the county five days a week. They requested only basic information and required no insurance, social security number or other details that might discourage people from getting tested.
By spring, the team was offering vaccinations too. They shifted to unconventional sites, such as Monument Crisis Center, Concord Flea Market and shopping center parking lots, meeting the community where they were. They vaccinated as many as 350 and tested up to 100 people per week. Many were from unhoused, uninsured, low income and minority communities. Currently, they administer about 90 tests and 200 vaccines per week.
“La Clinica stepped in as a trusted community organization, provided access to some of the hardest-to-reach populations, and started a dialogue to build trust again with health service agencies,” she said.
Laurie Flaherty, MS ’92  Laurie Flaherty
Laurie Flaherty
Laurie Flaherty, coordinator of the National 911 Program since 2004, served as the 911 subject matter expert to the Prehospital Working Group of the federal COVID Healthcare Resilience Task Force. The collaboration between the National 911 Program and the task force produced multiple resources to assist 911 organizations during the pandemic, including guides on leveraging telemedicine practices and maintaining the capability to continue mission-critical functions to support first responders and the community.
Flaherty’s work had an international impact as the “Continuity of Operations Response Plan,” which was developed with the 911 Program’s support, was translated into Spanish and shared with the Organization of America States’ 35 member countries. 911 plans for continuity of operations had been created to deal with issues such as natural disasters and power outages, but this was the first plan to address infectious disease outbreaks.
 Annesa Flentje Annesa Flentje, PhD, Assistant Professor
Annesa Flentje Annesa Flentje, PhD, Assistant Professor
Annesa Flentje is examining the health effects that LGBTQ+ individuals are experiencing from COVID-19. She is a UCSF researcher who joined the We Count Collaborative, a nationwide research and data-sharing project providing health data on 45,000 LGBTQ+ individuals. The initiative’s goal is to bridge the gap in knowledge about COVID-19 health experiences, including rates of infection and outcomes, for LGBTQ+ people. The We Count Collaborative is partnering with The PRIDE Study, a national longitudinal study of LGBTQ+ individuals and other gender and sexual minorities. Flentje, who serves as The PRIDE Study’s associate director, plans to track the mental and physical health of participants for years to determine if the pandemic has lasting effects.
Elizabeth Gatewood, DNP, MS ’08, FNP, Assistant Dean  Elizabeth Gatewood
Elizabeth Gatewood
As the UCSF School of Nursing’s new Assistant Dean for Education Technology Innovation in February 2020, Elizabeth Gatewood planned to spend four months developing a plan for growing the School’s use of technologies to enhance students’ academic learning. Then came COVID-19. In mid-March, California Gov. Gavin Newsom issued a statewide stay-at-home order, forcing schools, employers and other organizations to transition to remote working and learning.
Gatewood immediately set to work transitioning the School’s academic programs and its faculty and students to remote education — and fast. Gatewood and her team helped train faculty on how to deliver coursework remotely. They adopted videoconferencing, telehealth, virtual patient simulation software and other technologies. Then, they shared what they learned with colleagues across the campus. Their efforts ensured that nursing students remained engaged and continued their academic progress uninterrupted.
 Kristen Harknett Kristen Harknett, PhD, Associate Professor
Kristen Harknett Kristen Harknett, PhD, Associate Professor
Kristen Harknett has shined a spotlight on the country’s 25 million service industry workers whose lives have been heavily impacted during the pandemic. Many were laid off or faced reduced work hours. Some who were deemed essential workers, such as grocery and pharmacy workers, continued working but risked exposure to COVID-19 whenever they came to work. Many service workers came to work ill because they are not offered paid sick leave and cannot afford to lose a day’s wages.
Harknett and her colleagues at The Shift Project have published multiple studies, testified before government agencies, and spoken with reporters to help lawmakers, employers and the public understand the importance of paid sick leave. Some of their recent findings were reported in an August article in Health Affairs titled “Olive Garden’s Expansion Of Paid Sick Leave During COVID-19 Reduced The Share Of Employees Working While Sick.”
Charlene Harrington, PhD, RN, FAAN, Professor Emerita, and Susan Chapman, PhD, RN, FAAN, Professor  Charlene Harrington, Susan Chapman
Charlene Harrington, Susan Chapman
Charlene Harrington and Susan Chapman have played significant roles in bringing to light the adverse impacts of COVID-19, especially on some of the nation’s most vulnerable individuals. Along with School of Nursing colleagues including Leslie Ross and Elizabeth Halifax, they found that California nursing homes with RN staff levels below recommended levels were twice as likely to have COVID-19 resident infections. Their findings emphasize the need for establishing and enforcing minimum staffing standards at the federal and state levels to assure resident safety and quality care.
Harrington also co-authored a report commissioned by the California Health Care Foundation, investigating COVID-19’s impact in nursing homes. In addition, Chapman and School of Nursing faculty member Laura Wagner examined staffing in alternative care settings in California and other states and studied the challenges of rural home care workers during COVID-19.
 Orlando Harris Orlando Harris, PhD, MPH, FNP, Assistant Professor
Orlando Harris Orlando Harris, PhD, MPH, FNP, Assistant Professor
As an expert peer review panelist for the national COVID-19 Prevention Network, Orlando Harris reviews federal-sponsored COVID-19 vaccine efficacy trial protocols and makes recommendations on the significance, impact and ethics for the Black community.
Harris has worked to enhance understanding of vaccine hesitancy by creating the conceptual framework, “The Stages of COVID-19 Vaccine Readiness and Acceptance.” Through his research, he is studying COVID-19’s impact on communities of color, and the impact of medical mistrust and racism on vaccine uptake.
He helped advance vaccination efforts by collaborating with the UCSF Pandemic Initiative for Equity and Action to create a program that has trained over 11,500 public health workers in vaccination outreach statewide. He participated in Kaiser Family Foundation’s campaign, “The Conversation,” which provided the Black community with credible information about vaccines.
“Ensuring equitable access to the vaccines is at the core of public health nursing practice,” he said.
Jennifer James, PhD (’16), MSW, MSSP, Assistant Professor  Jennifer James
Jennifer James
Jennifer James has worked to detail the experiences of Black birthing people and Black birthworkers during the pandemic. Her March 2021 publication gave voice to the challenges birthworkers faced due to the intersection of COVID-19 restrictions and structural racism. She highlighted the innovative strategies used to support Black birthing people in the pandemic and beyond.
James is also examining the implications of the pandemic for incarcerated women over age 50 with chronic illnesses. She has interviewed women released from California prisons and jails during the pandemic, as well as correctional health care providers, and advocates and organizers supporting decarceration efforts. She has a paper under review that describes the mental health implications of COVID-19 risk mitigation strategies in California’s women’s prisons and several papers in preparation that elucidate carceral experiences of COVID-19 in California prisons and jails.
 Monica McLemore Monica McLemore, PhD (’10), RN, Associate Professor
Monica McLemore Monica McLemore, PhD (’10), RN, Associate Professor
Monica McLemore is leading innovative research examining COVID-19’s impact on pregnant people, especially people of color. With funding from the Robert Wood Johnson Foundation, she helped launch Research Priorities of Affected Communities (RPAC), a research protocol centered on women with high sociodemographic risk for pre-term birth. McLemore’s team partnered with seven community-based organizations to hold 12 RPAC sessions across the U.S. The team is studying how health care facilities treated Black, Indigenous and People of Color (BIPOC) individuals who had or were suspected to have COVID-19. They also are assessing the lack of resources for people living in rural communities who contracted COVID-19 and had other comorbidities or were immunocompromised.
In addition, McLemore continues to lead the Reproductive Health Equity and Birth Justice CORE, an adjunct study to the PRIORITY pregnancy registry study, aiming to help patients and health care providers better understand how COVID-19 impacts BIPOC pregnant people and their newborns.
Van Ta Park, PhD, MPH, Professor  Van Ta Park
Van Ta Park
Van Park is leading multiple studies to enhance our understanding of the impact of COVID-19 on the Asian American and Pacific Islander (AAPI) community. She is the principal investigator for COMPASS, the first national multi-lingual study of its kind that is examining COVID-19 related discrimination, vaccine willingness, and issues around health care, caregiving and social support in AAPIs.
Her goal is to help inform policies and programs that will help alleviate the pandemic’s effects on the AAPI community. Early findings from COMPASS include: 76% of over 1,600 survey respondents had concerns about the COVID-19 vaccine; of the estimated 5,000 survey respondents, three in five reported experiencing some form of discrimination during the pandemic, and 59% believed the U.S. has become more dangerous for their ethnic group. UCSF colleagues Bora Nam, Linda Park and Marian Tzuang are also part of the COMPASS team. Several key findings were presented to professional networks and national audiences, and shared with the Congressional Asian Pacific American Caucus before a hearing regarding anti-Asian hate at the federal Capitol.
 Stephen Perez Stephen Perez (MS ’08)
Stephen Perez Stephen Perez (MS ’08)
Stephen Perez served as an Epidemic Intelligence Service Officer with the Centers for Disease Control (CDC) and Prevention during the pandemic’s early stages. Assigned to the New Jersey Department of Health, Perez developed policies and guidance for area health care facilities and investigated COVID-19 outbreaks throughout the state. He later transferred to CDC headquarters in Atlanta, where he serves as a nurse epidemiologist with the Outbreak Response Team within the Detection and Response Branch at the CDC's Division of HIV Prevention. As an officer in the U.S. Public Health Service, Perez was also deployed to serve as part of the CDC's COVID-19 response, including in the role as clinical lead for CDC's Vaccine Confidence Team where he led initiatives to improve vaccine uptake among health care workers. He also conducted national presentations, served as a liaison between multiple professional organizations, academic institutions and the CDC, and produced educational materials for nurses and other health care professionals.
Elena Portacolone, PhD (’11), MBA, MPH, Assistant Professor  Elena Portacolone
Elena Portacolone
Elena Portacolone has examined the impact of the pandemic on diverse older adults living alone with cognitive impairment in the San Francisco Bay Area. Collaborating with Julene Johnson, the School’s associate dean for research, and others, Portacolone’s study highlighted the fear, extreme isolation and misinformation this population has endured during the pandemic. Findings also underscored limited access to services, as well as the importance of home care aides. Portacolone has also written about the potential use of robots and other technologies to connect with underserved and vulnerable populations during times like a pandemic where isolation can be severe.
“The COVID-19 pandemic is showing us the urgency of interdisciplinary collaborations that ensure that emerging technologies clearly serve and protect users’ values and lives,” Portacolone said.
 Glenn-Milo Santos Glenn-Milo Santos, PhD, MPH, Associate Professor
Glenn-Milo Santos Glenn-Milo Santos, PhD, MPH, Associate Professor
Glenn-Milo Santos has published three studies in 2021 that are some of the first global studies to document the wide range of negative effects of COVID-19 among gay, bisexual and other men who have sex with men (MSM) worldwide. Examining more than 10,000 individuals across 20 countries, Santos discovered these individuals lacked access to HIV prevention and treatment services, experienced negative economic and mental health impacts, and those who practiced physical distancing felt more lonely and anxious. These harmful effects were even more evident among MSM from historically marginalized groups (e.g., racial minorities, immigrants, and socioeconomically disadvantaged MSM).
“These findings highlight the urgent need to mitigate the negative impacts of COVID-19 among MSM globally, particularly those with intersecting vulnerabilities,” Santos said.
His team also recently completed a follow-up study to more deeply examine COVID-19’s persistent negative impacts among an additional 22,000 participants. The manuscript is under peer review.
Gina Shuler, PhD ’13, RN, Chief Population Health Officer for UCSF Health; Associate Dean, UCSF School of Nursing  Gina Shuler
Gina Shuler
As COVID-19 struck in early 2020, Gina Shuler led the charge to open UCSF hotlines for patients and employees. Health care experts, including nurse practitioner students from the School of Nursing, fielded hundreds of calls a day, screening people for COVID-19, connecting them with the appropriate level of care, and educating them about how to obtain testing or effectively quarantine. Shuler has operational oversight of the COVID Results Information & Short-Term Monitoring Program (CRISM) nursing team, a specialized team that monitors and connects COVID-positive patients to needed care.
As an executive leader of UCSF’s occupational health COVID response team, along with the chief medical and chief innovation officers, Shuler helped manage the screening, testing, contact tracing and “return to work” management for UCSF’s entire employee population. With the arrival of COVID vaccines in December 2020, Shuler co-led the university’s multi-phased vaccination program, including the rollout of the vaccines to highest priority groups first and the opening of multiple vaccine clinics where more than 250,000 vaccines have been administered.
 Merry Taheri Merry Taheri, DNP ’19, RN, NP-C
Merry Taheri Merry Taheri, DNP ’19, RN, NP-C
During the pandemic, Merry Taheri managed three Los Angeles-area COVID-19 isolation and quarantine (IQ) sites, including the 245-bed Sheraton Hotel in Pomona — the largest IQ site in the nation — as a clinical commander of Los Angeles County’s Department of Health Services. She oversaw the welfare of more than 2,000 COVID-19 patients during this time. Taheri hired over 300 health care professionals to staff the sites, advised on care protocols, oversaw multi-million dollar budgets and even found time to examine patients, among her many duties.
Her work did not go unnoticed. The Service Employees International Union (SEIU) appointed her to the SEIU Healthcare Worker COVID Advisory Committee, which continues to advise the Biden-Harris COVID Task team. Taheri also created a consulting firm specializing in COVID-19 services, such as implementing protocols, policies and testing for schools, film productions, businesses and private events.
Jian Zhang, DNP, MS ’92, FAAN  Jian Zhang
Jian Zhang
As CEO of Chinese Hospital in San Francisco’s densely populated Chinatown, Jian Zhang helped mobilize health and safety practices in the community at the very start of the pandemic to successfully prevent a COVID-19 outbreak in the Chinatown district.
Since January 2020, Zhang has been leading Chinese Hospital to safeguard the community through the pandemic. In addition to elevating its Emergency Department to Basic Services to receive sicker patients and expanding bed capacity to help Zuckerberg San Francisco Hospital, Zhang led the implementation of a comprehensive COVID-19 initiative consisting of bilingual community education and outreach, testing, contact tracing, quarantine, linkage of care and vaccination, in collaboration with the San Francisco Department of Public Health, elected officials and community leaders. These prevention and mitigation efforts have proven successful, as the Chinatown community remains one of the areas with very low infection rates, despite being one of the most densely populated areas in the nation.



