
Jim Stotts (photo by Elisabeth Fall)
A Voyage Without a Map: Improving Alarm Safety at UCSF Medical Center
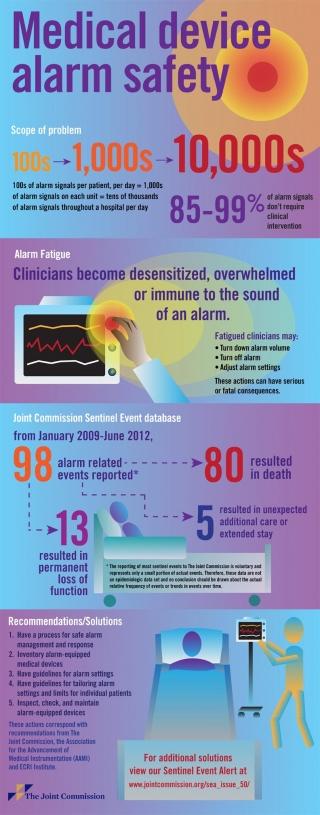
In 2014, a study led by UC San Francisco School of Nursing’s Barbara Drew found that 461 patients across five adult intensive care units at the UCSF Medical Center generated an astounding 2.5 million alarms in just 31 days. It was the largest study of its kind, adding to an increasing body of evidence suggesting that alarm fatigue – desensitization to the sounds and alerts that continually bombard clinicians in acute care settings – is a significant patient safety problem.
The same year, the Joint Commission (the independent nonprofit organization that accredits hospitals and other health care organizations in the US) added a new national patient safety goal requiring hospitals to prioritize alarm system safety, identify the most important alarms and, beginning in 2016, develop policies and procedures to manage them.
A New Committee to Examine Alarm Safety
 As patient safety manager, Jim Stotts coordinated the UCSF Medical Center’s activities to address the Joint Commission mandate. He says that in the past, responsibility for alarm management issues was decentralized. Questions were often directed to individuals with specific expertise. “There was no central group accountable for ensuring practice consistency across the UCSF Health enterprise,” he says.
As patient safety manager, Jim Stotts coordinated the UCSF Medical Center’s activities to address the Joint Commission mandate. He says that in the past, responsibility for alarm management issues was decentralized. Questions were often directed to individuals with specific expertise. “There was no central group accountable for ensuring practice consistency across the UCSF Health enterprise,” he says.
But decisions about alarm management affect many areas in the hospital, including the emergency department, acute care and critical care, and may differ depending on setting, purpose, and age of the patient. With more units gaining the capacity to do telemetry monitoring, it made sense to engage stakeholders from across the medical center to look at alarm management issues and formulate guidelines and revise policies.
Stotts and representatives from across several disciplines and departments, including nursing, medicine, clinical engineering, information technology, respiratory therapy and materials management, formed the Clinical Alarm Management (CALM) Committee to examine and improve how alarms are managed and to meet the Joint Commission’s new alarm safety goals.
On the surface, their task may seem simple: figure out which alarms, parameters and practices don’t contribute to safety and good patient care, and discontinue or change them. But a lack of good data and conflicting guidelines, coupled with both human and technological challenges, make it surprisingly difficult to find the sweet spot between too much and too little information.
Electrode Management
Skin electrode management is one example of a practice issue that is more complicated than it might seem to the casual observer. Electrodes – the small pads that are attached to the patient’s chest and have lead wires that send signals to the monitor – can wear out and compromise signal quality, sometimes resulting in false alarms.
But what’s the best interval for changing them, storing them or discarding unused electrodes?
“While there’s anecdotal data to suggest that electrodes should be changed every 24 hours, there’s very little research-based experimental data to support that,” says Michele Pelter, assistant professor of physiological nursing and director of the ECG Monitoring Lab (formerly the Drew Lab), who studies heart disease and monitoring, and serves on the CALM Committee.
Moreover, there are conflicting recommendations on when to discard electrodes after opening the package. The medical center’s current vendor recommends a maximum of 72 hours, while the Joint Commission’s informal recommendation is 30 days, says Stotts.
Without fully vetted guidelines, UCSF policy for inpatient monitoring is to change electrodes every 48 hours or as needed if there is poor signal quality. The hospital is moving toward endorsing hospital units that don’t use electrodes very often – such as some ambulatory care units – moving away from using bulk-packaged electrodes to avoid the risk of poor signal quality caused by older electrodes from previously opened packages.
Alarm Parameters
The CALM committee is also grappling with the difficult issue of alarm parameters – the software settings that determine when, and what kind of, alarms are sent.
With researchers from the School of Nursing, they looked at patient data to determine if there was any low-hanging fruit – parameters that could be changed to reduce alarms without jeopardizing patient safety. Using the Drew study, they made modifications to parameter settings for oxygenation and arrhythmia monitoring in adult patients. A re-examination of monitoring in the adult ICUs a year later did not show any additional sources for improvement. The UCSF research group continues to mine the data for opportunities.
At UCSF Benioff Children’s Hospital San Francisco, clinical informatics specialist Kevin Spolini, also a member of the CALM Committee, is using the data to make adjustments to alarm parameters and modifying the type, volume and frequency of alarms sent to nurses’ phones to reduce the number of nuisance alarms.
It’s clear, says Pelter, that there are significant improvements to be made in monitoring software that could reduce false alarms. “Their algorithms are so sensitive, they alarm too often,” she says.
One of her current research projects looks at signals called low-amplitude (also known as low-voltage) QRS – heart rhythms that don’t generate tall waveforms on an electrocardiography (ECG) monitor and appear to be one cause of false alarms. As a safety measure, the monitoring software requires rhythms to generate tall waveforms, often from multiple leads, in order to be counted as heartbeats. But there are several reasons, including obesity or prior heart disease, that some leads may result in low-amplitude QRSs and may not be an indicator of an acute problem requiring intervention.
Pelter believes the software manufacturers may have opportunities to help reduce false alarms. “Some of the issues are software related, but at the moment, the burden is on nurses,” she says.
Why Do Some Patients Generate Multiple Alarms?
Of course, it’s tricky to create algorithms that address every situation that can arise among a highly variable patient population with a host of different conditions and needs.
 Xiao Hu, Michele Pelter, Richard Fidler
Xiao Hu, Michele Pelter, Richard Fidler
The medical center/School of Nursing project that examined alarms also found that a subset of patients seems to generate the majority of alarms. “The question is, what is it about those patients, and what can we do to address those alarms?” says Stotts.
“The patients generating most of the alarms are probably people with cardiac pathology that has altered their waveforms,” says Pelter. Conditions like long-standing hypertension, prior heart attacks, implanted pacemakers and, possibly, obesity or lung disease may contribute. But to the monitor, a concerning waveform is a concerning waveform, regardless of the individual patient’s condition.
“It gets confused,” says Pelter. “The patient’s baseline is normal for them, but the algorithm thinks it’s a bad arrhythmia.”
Pelter, along with the School’s Xiao Hu and Richard Fidler, are working on a proposal in collaboration with the medical center that would enlist nurses and physicians to capture data on individual alarms. The data could generate a regular report that might be used on daily rounds to adjust alarm settings based on individual patients’ needs.
Reconciling Alarm Standards and Physicians’ Orders
The CALM Committee is also addressing conflicts between physicians’ orders and standard alarm parameters. Stotts says, “We’ve found that our order writing isn’t always compatible with how we’re setting our machines.” For example, the standard setting for oxygen saturation generates an alarm when it falls below 88 percent, but physicians often write a different parameter in their orders. “We’re trying to understand the deviations,” says Stotts.
Filling In the Research Gaps
Stotts and Pelter agree that there is no simple road map to increasing alarm safety. Health care organizations are under pressure to improve, but no one is giving any specific direction. Research demonstrates that alarm fatigue is a problem, but there’s little research yet on how to safely address it. Pelter says, “It seems like regulatory agencies are saying, ‘OK, you hospitals, fix this,’ but this problem is so new they can’t give us any criteria [for success].”
Researchers like Pelter are trying to fill in the gaps. With an international group from the Society of Critical Care Medicine, she and Xiao Hu are working on a Gordon and Betty Moore Foundation-funded grant to do an in-depth literature review, which they hope will yield evidence-based strategies for alarm management.
Pelter is also working with medical center clinical nurse specialist Cass Sandoval on a grant from the American Association of Critical-Care Nurses to drill down further into the data Barbara Drew collected to look at the group of alarms that were true but turned out to be not clinically actionable. “We don’t treat [those arrhythmias]; we don’t change care,” says Pelter. “Our hope is that we can ultimately make recommendations to monitoring companies on reducing nonactionable alarms.”
Until there is a more robust evidence base for what works, those responsible for alarm safety have to walk a careful line between doing too much and doing too little. The UCSF Medical Center has met the Joint Commission’s goal for 2016, but there’s much more to be done, and it will require collaboration among researchers, bedside clinicians, engineers and technology organizations. Stotts says, “It’s helpful having people who care about it look at it in a thoughtful way. We’re figuring it out together.”



