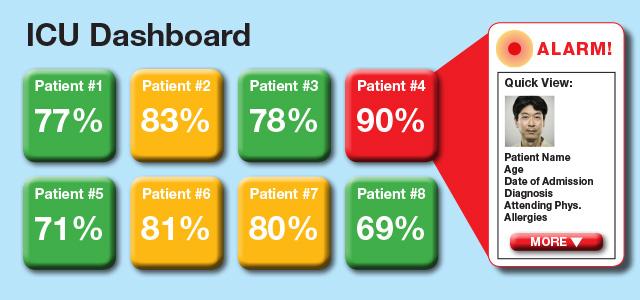
The proposed super alarm might have a dashboard that looks something like the above graphic. This dashboard displays a numeric score, which the super alarm algorithm generates and which represents the probability of risk for a patient.
“Nerds and Nurses” Race to Develop Super Alarm to Combat Alarm Fatigue
The technology in a hospital intensive care unit (ICU) is extraordinary in its ability to pick up the slightest alterations in bodily functions and recognize when they slip out of the “normal” range. But as most ICU nurses understand all too well, having all of that clinical information does not always translate into improvements in patient care.
For one, despite their remarkable sensitivity, ICU monitors still miss some critical clinical events, in part because they cannot adequately synthesize disparate data points to give clinicians appropriate early warnings. Equally important, a UCSF study found that there were 187 audible alarms per bed per day in the ICU, with a false-positive rate of over 88 percent for arrhythmia alarms. Put that in the context of other noise in the ICU and all of the other duties nurses must perform, and you begin to understand the concept of alarm fatigue. It’s no surprise that in many settings, clinicians ignore alarms, turn them down or turn them off, leading to a nationwide epidemic that goes beyond the ICU to other hospital units.
It also explains why an interdisciplinary team of UC San Francisco researchers, led by Xiao Hu, Michele Pelter and Richard Fidler from UC San Francisco School of Nursing, is working furiously to create and test a “super alarm.” This device would aggregate disparate data, capture trending patterns and filter out false alarms, so clinicians are, in theory, only and always alerted when there is a situation that truly demands clinical attention.
The team has already shown they can achieve 90 percent sensitivity in predicting ICU cases where a patient is in need of resuscitation – known in hospitals as code blue – and is on track to complete a prospective National Institutes of Health (NIH)-funded clinical study by the end of 2017.
Effective Collaboration
 Xiao Hu, Michele Pelter, Richard Fidler To achieve their aims, the team jokes they’ve formed a powerful alliance “between nurses and nerds.” Hu is a biomedical engineer, Pelter is a critical care nurse who leads the ECG Monitoring Research Lab at the School, and Fidler is an assistant adjunct professor in the School of Nursing, a critical care nurse practitioner and a nurse anesthetist who has a clinical simulation lab at the San Francisco VA Health Care System (SFVA) that tests the usability of medical technology. They have assembled a group of like-minded clinicians and IT experts to develop their super alarm.
Xiao Hu, Michele Pelter, Richard Fidler To achieve their aims, the team jokes they’ve formed a powerful alliance “between nurses and nerds.” Hu is a biomedical engineer, Pelter is a critical care nurse who leads the ECG Monitoring Research Lab at the School, and Fidler is an assistant adjunct professor in the School of Nursing, a critical care nurse practitioner and a nurse anesthetist who has a clinical simulation lab at the San Francisco VA Health Care System (SFVA) that tests the usability of medical technology. They have assembled a group of like-minded clinicians and IT experts to develop their super alarm.
“As clinicians, we need computer geeks, because they present possibilities we would never have considered – a lab value that at first we may think nothing of, but in combination with an ECG [electrocardiography] rhythm, may matter,” says Fidler. “And they need us, because we’ll ask why can’t we capture certain measures that we know are clinically important.”
For example, Hu’s expertise in signal processing and machine learning enables him to design tools that get thorough and accurate information from the body’s “signals” and to generate or modify alarm algorithms based on changing data inputs. In theory, the super alarm will use these processes to recognize clinically important patterns more quickly and with more reach than is humanly possible, while filtering out irrelevancies – those little bits of information that don’t mean anything when they come together as part of a big pattern, but which today set off all those false-positives.
“It is, in a sense, what nurses do in the ICU – they’re watching things all the time, recognizing trends – but with all the data we have these days, including from EHRs [electronic health records], we don’t always have the human bandwidth to filter, synthesize and recognize when the pattern indicates real clinical urgency,” says Pelter. “So engineers grab these data points, and we ground them in who cares and what matters.”
Stage One: Doing Better on Predicting and Avoiding Code Blue
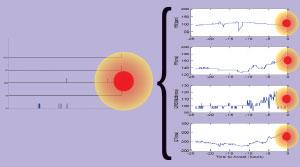 On the left side, this patient, who suffered a cardiac arrest, didn’t have many alarms at all over the prior 12-hour period, but more precise monitoring of several ECG metrics that are not currently available on patient monitors (seen on the right) could have alerted staff earlier and possibly detected this patient’s deterioration approximately six hours prior to cardiac arrest. Initially, the team focused its attention on better predicting and averting code blue cases, in the hope, says Fidler, “that it would allow us to be right a higher percentage of the time, so we can save more lives.”
On the left side, this patient, who suffered a cardiac arrest, didn’t have many alarms at all over the prior 12-hour period, but more precise monitoring of several ECG metrics that are not currently available on patient monitors (seen on the right) could have alerted staff earlier and possibly detected this patient’s deterioration approximately six hours prior to cardiac arrest. Initially, the team focused its attention on better predicting and averting code blue cases, in the hope, says Fidler, “that it would allow us to be right a higher percentage of the time, so we can save more lives.”
They found they could use the technology to identify patterns that until now have remained obscure: individualized patient values that change over the two to three hours prior to a patient having a heart attack or losing his or her ability to breathe.
“We found, for example, that PR intervals slowly increase before a cardiac arrest,” says Hu. “When we presented that to clinical folks, they agreed that it makes sense physiologically.”
Testing the Results, Expanding the Focus
Having shown that the alarm can predict code blue cases hours ahead of time with reasonable accuracy, the group is running the NIH-funded study to complete more comprehensive testing of the super alarm in UCSF ICUs. The super alarm will run in the background while everyday clinicians simultaneously monitor patients using today’s standards of care.
“The challenge is to show that this approach works better for more patients, so we need a baseline to see what types of things we’re currently missing,” says Fidler. “The study is testing whether we can proactively and prospectively predict code blue events and get an actionable alarm that is not a nuisance and does not contribute to alarm fatigue.”
To that end, the group has engaged a professional design firm to create a user-friendly, front-end interface for the nursing station and mobile devices.
“We hope that this is only a starting point to develop an approach for other conditions – such as neurological deterioration, sepsis, hemorrhage and acute respiratory failure – as well as other parts of the hospital, outside of the ICU,” says Pelter.
“For a lot of these conditions, we may not have the patient data yet to do a good job, and might need to add additional data modalities, like tissue perfusion or gene expression data,” says Hu. “We won’t know until we start doing this, but we are excited by the possibilities.”



